Have you ever thought about getting insurance to cover diastasis recti surgery? This condition causes your abdominal muscles to separate. Many people face financial challenges when trying to treat it.
But, there’s hope. Insurance might cover your diastasis recti repair. In this guide, we’ll show you how to increase your chances of getting it covered.
But first, let’s ask a key question. When is diastasis recti seen as a medical need, not just a cosmetic issue? Knowing this can help you get insurance to cover your treatment. Let’s explore diastasis recti, its health impacts, and how to get insurance approval.
Key Takeaways
- Understand the medical criteria for diastasis recti surgery to be considered a necessity by insurance providers.
- Learn how to effectively document your condition and the need for surgical intervention.
- Discover the various types of insurance coverage available for abdominal wall reconstruction procedures.
- Develop a plan to work closely with your healthcare team to secure insurance approval.
- Explore alternative financing options if insurance coverage is denied.
Understanding Diastasis Recti and Its Medical Impact

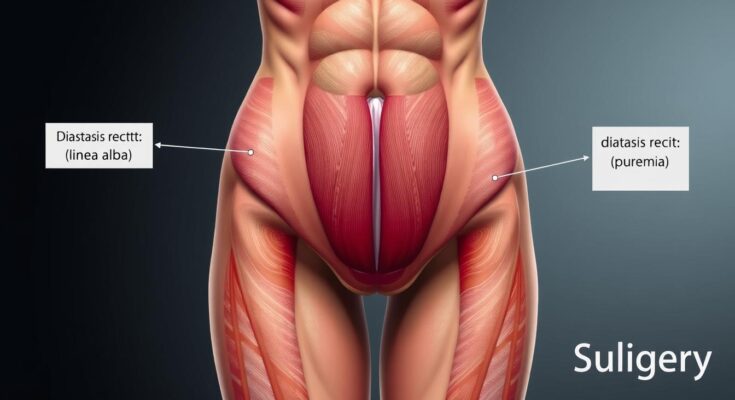
Diastasis recti is when your abdominal muscles separate. This can happen during pregnancy or after certain surgeries. It can lead to many problems that might need surgery to fix.
Common Symptoms and Complications
People with diastasis recti might feel lower back pain and pelvic instability. They could also have trouble controlling their urine or get hernias. The separated muscles can make the belly bulge out, which is hard on the body and mind.
Also Read: Protect Your Business with Key Man Disability Insurance.
When Surgery Becomes Medically Necessary
Sometimes, surgery is needed for diastasis recti. This is true if the muscles separate so much that it’s hard to move or exercise. If hernias or other serious problems come from it, surgery is often a must.
| Condition | Symptoms | Potential Complications |
|---|---|---|
| Diastasis Recti |
|
|
“Diastasis recti is a common condition that can have significant medical consequences, and understanding its symptoms and complications is critical for determining when surgical intervention may be necessary.”
How To Get Diastasis Recti Surgery Covered By Insurance
Getting insurance to cover diastasis recti surgery can be tough. But, with the right steps, you can boost your chances. It’s all about understanding what your insurance needs and showing them with solid proof.
Start by working closely with your doctor to prove the surgery is needed. You’ll need to show how the diastasis recti affects you. This could be through chronic back pain, bad posture, or trouble with daily tasks.
- Collect medical records, like CT scans or MRI images, to show how big the diastasis recti is.
- Get a detailed letter from your doctor or surgeon. It should explain why you need the surgery, including your symptoms and how they limit you.
- Keep track of any treatments you’ve tried first, like physical therapy or exercises, that didn’t work.
Once you have all your documents in order, it’s time to ask for insurance coverage for abdominoplasty. You’ll need to give a full report on your condition, the surgery plan, and what you hope to achieve.
Insurance companies look at each case differently. So, it’s key to make a strong case for why you need the surgery. With help from your healthcare team and solid evidence, you can get the insurance coverage you need.
“The key to securing insurance coverage for diastasis recti surgery is to clearly demonstrate the medical necessity of the procedure.”
Documenting Medical Necessity for Insurance Approval
To get insurance for diastasis recti surgery, you need to show it’s medically necessary. This means you’ll need to gather medical tests, imaging, doctor’s statements, and physical therapy records.
Required Medical Tests and Imaging
Insurance companies want to see certain tests to decide if surgery is needed:
- An ultrasound or CT scan to measure the diastasis and check the abdominal wall.
- Functional tests, like the Valsalva maneuver, to see how the diastasis affects daily life.
- Tests to check muscle strength and range of motion to see how much it’s affecting you.
Physician Documentation Guidelines
Doctors need to write detailed notes to support your claim. They should include:
- A full physical exam, measuring the diastasis and any related issues.
- How the diastasis affects your daily activities, like core stability, back pain, or pelvic floor problems.
- Any non-surgical treatments tried, like physical therapy or binders, and if they worked.
- Why surgery is needed to fix the abdominal wall and improve your life.
Physical Therapy Records
Insurance also wants to see if you tried non-surgical treatments first. This usually means physical therapy records. These should have:
- Details of your physical therapy plan, including exercises for the diastasis.
- Updates on how you’re doing, and why you need surgery now.
- Measurements of the diastasis and any changes in your function during therapy.
By showing a strong case for needing surgery, you can boost your chances of getting insurance approval.
Also Read: How to Sell Pet Insurance Successfully | Expert Guide.
Different Types of Insurance Coverage for Abdominal Wall Surgery

Understanding insurance for surgeries like diastasis recti repair and pregnancy-related procedures can be tough. But knowing about different insurance policies and their rules can help you get the coverage you need.
One common policy that might cover tummy tuck surgery is the cosmetic and reconstructive surgery plan. This plan often helps with functional issues, like fixing diastasis recti. This is a muscle separation in the abdomen that can happen during pregnancy.
| Insurance Plan | Coverage for Abdominal Wall Surgery |
|---|---|
| Cosmetic and Reconstructive Surgery | May cover diastasis recti repair and other functional procedures |
| Maternity and Pregnancy-Related Care | Likely to cover abdominal wall surgeries connected to pregnancy complications |
| Hernia Repair | May include coverage for umbilical hernia repair, which can be combined with diastasis recti surgery |
Maternity and pregnancy-related care insurance plans might also cover abdominal wall surgeries. This is specially true for surgeries related to pregnancy issues, like diastasis recti. Some policies that cover hernia repair might also include umbilical hernia repair. This can often be done with diastasis recti surgery.
Understanding Your Insurance Policy
It’s important to carefully look at your insurance policy. Talk to your healthcare provider and explain why you need the surgery. This way, you can better understand your insurance options. Knowing about different coverage types can help you get the care you need.
Distinguishing Between Cosmetic and Medical Procedures
It’s important to know the difference between cosmetic and medical procedures for diastasis recti repair. Cosmetic procedures, like a standard abdominoplasty (tummy tuck), usually aren’t covered by insurance. But, if the repair is medically necessary, insurance might cover it.
Understanding Insurance Policy Language
Insurance policies have specific words to decide on coverage for abdominal surgeries. Words like “functional impairment,” “medical necessity,” and “activities of daily living” are important. Knowing these terms can help patients make a stronger case for coverage.
Combining with Umbilical Hernia Repair
Another way to get insurance to cover diastasis recti repair is to do it with an umbilical hernia repair. Umbilical hernias often come with diastasis recti. Insurers might cover both procedures because they fix a medical issue, not just for looks. This can help get approval for umbilical hernia surgery and insurance coverage for abdominoplasty.
“Combining diastasis recti repair with umbilical hernia surgery can strengthen your case for insurance coverage, as it demonstrates the medical necessity of the procedure.”
By understanding insurance policies and looking into combining procedures, patients can better get coverage for diastasis recti repair.
Also Read: Insurance of the Carolinas – Your Local Coverage Partner.
Working with Healthcare Providers for Insurance Authorization
Getting insurance for abdominal wall reconstruction can be tough. But, working well with your healthcare team can help a lot. A strong partnership with your surgeon and other doctors is key. This ensures your medical records show why you need the pre-approval requirements for abdominal wall reconstruction.
It’s important to talk openly with your healthcare team during the insurance process. Tell them about your insurance plan’s needs. Together, you can create a treatment plan that meets both your health needs and the insurer’s rules. Your doctors can also help fight for your case and make sure all needed documents are sent on time.
Collaborate with Your Providers
- Schedule regular check-ups and follow-up appointments to monitor your condition and document its progression.
- Discuss the pre-approval requirements for abdominal wall reconstruction with your healthcare team and work together to build a strong case for medical necessity.
- Ensure that your medical records clearly outline the severity of your symptoms, the functional limitations you experience, and the possible long-term consequences if the condition is left untreated.
By working closely with your healthcare providers, you can feel more confident in the insurance approval process. This can help you get the coverage you need for your pre-approval requirements for abdominal wall reconstruction.
“Effective communication and collaboration with your healthcare team is key to getting insurance authorization for medically necessary procedures like abdominal wall reconstruction.”
Navigating the Insurance Appeals Process
Getting your diastasis recti surgery covered by insurance can be tough. But don’t give up. If your claim is denied, you need to appeal. This means writing a strong appeal letter and gathering solid evidence to support your case.
Writing an Effective Appeal Letter
A successful appeal needs a clear and strong argument. Your appeal letter should cover a few key points:
- A brief summary of your condition and why surgery is needed
- An explanation of how the surgery fits the insurance policy’s medical necessity criteria
- References to medical studies and test results that back your claim
- A request for a full review of your claim
Gathering Supporting Documentation
You’ll also need to collect a lot of supporting documents. These might include:
- Copies of all your medical records, like doctor’s notes and test results
- A detailed letter from your surgeon explaining why surgery is necessary
- Photos or other visual proof of your diastasis recti
- Any relevant medical research or literature that supports your surgery
By following these steps and fighting for your case, you can improve your chances of getting insurance coverage for your diastasis recti surgery.
Alternative Financing Options and Payment Plans
If you’re having trouble getting insurance for diastasis recti surgery, don’t worry. There are other ways to pay. You can look into medical credit cards for flexible financing. Some healthcare providers also offer payment plans to help spread out the cost.
Some patients might qualify for financial help from hospitals, non-profit groups, or even the surgery team. These programs can reduce the cost of surgery. It’s key to look into these options to see if they can help.
Don’t forget to talk to your healthcare provider about the cost. They might be able to offer discounts or payment plans that fit your budget. By exploring these options, you can get the treatment you need for diastasis recti.
FAQ
How can I get my diastasis recti surgery covered by insurance?
To get your diastasis recti surgery covered, show it’s medically necessary. You’ll need a letter from your doctor explaining your condition and why surgery is needed. Follow your insurance’s rules and appeal if they say no.
What is diastasis recti and when is surgery medically necessary?
Diastasis recti is when your belly muscles split, often during pregnancy. It can make your belly bulge, hurt your back, and affect your pelvic floor. Surgery is needed if other treatments don’t work or if the split is very big.
What documentation is required to prove medical necessity for diastasis recti surgery?
To prove you need surgery, you’ll need a detailed medical record. This includes test results, doctor’s notes, and proof of trying physical therapy. Your doctor can tell you what else you need.
How can I appeal a denied claim for diastasis recti surgery?
If your claim is denied, you can appeal. Write a letter explaining why you need surgery and add any extra proof. Make sure to follow your insurance’s appeal process closely.
What are the out-of-pocket costs for diastasis recti surgery if my insurance doesn’t cover it?
The cost of surgery without insurance can be high. It can be between $5,000 and $15,000 or more. If you can’t get insurance to cover it, look into financing options or payment plans.